Abstract
On behalf of the GRAALL group.
Introduction. Tyrosine kinase inhibitors (TKIs) have dramatically improved the outcome of patients diagnosed with Philadelphia chromosome (Ph)-positive acute lymphoblastic leukemia (ALL). In a previous randomized trial (GRAAPH-2005; Chalandon Y., Blood 2015), our group demonstrated that anthracycline and cyclophosphamide could be safely omitted during the first Hyper-CVAD chemotherapy cycle when combined to imatinib. In the present GRAAPH-2014 trial, we investigated whether the use of nilotinib, a 2 nd generation TKI, would allow further decreasing chemotherapy intensity through the omission of high-dose cytarabine (HD-AraC) during consolidation cycles 2 and 4.
Methods. From March 2016, patients aged 18-60 years old were randomized frontline to receive 4 cycles (1=3, 2=4) of chemotherapy combined with continuous nilotinib 400 mg bid. Cycle 1 and 3 were similar in both arms, identical to the less-intensive first cycle of the previous GRAAPH-2005 trial with weekly vincristine and dexamethasone and nilotinib instead of imatinib. Cycle 2 and 4 differed between control arm A (MTX 1 g/sqm over 24h, HD-AraC 3 g/sqm/12h for 2 days) and experimental arm B (MTX 1 g/sqm over 24h only). Marrow minimal residual disease (MRD) was assessed by both BCR-ABL1 and IG-TCR qPCR after each cycle (MRD1-4). Patients in complete remission (CR) after cycle 4 were eligible to receive allogeneic stem cell transplant (alloSCT). Non allografted patients had the option to receive autologous SCT (autoSCT) if a major molecular response (MMolR) (MRD4 BCR-ABL1 <0.1%) was achieved. AlloSCT and autoSCT were followed by a 2-year imatinib maintenance. The randomization was stratified on age (≤40y, >40y) and BCR-ABL1 breakpoint region (M/m-bcr). MMolR rate at MRD4 was the primary endpoint of this non-inferiority study, with a margin set at 0.15. In February 2019, the study DSMB decided to stop the randomizations after an unplanned analysis demonstrating a significant excess of relapse in arm B (without HD-AraC). An intention-to-treat analysis is provided. All patients gave informed consent. The study is registered at EudraCT under the number: 2014-002146-44.
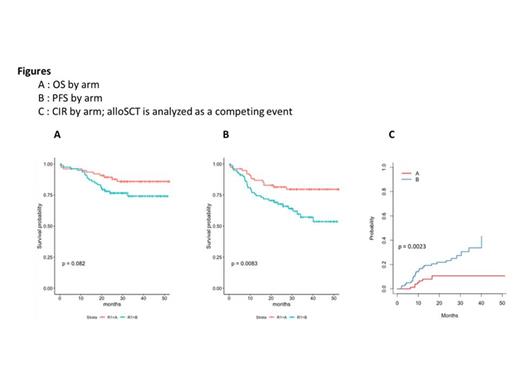
Results. A total of 156 patients were randomized (77 in arm A, and 79 in arm B). Median age was 47.1 years old (range 18.1-59.9). One-hundred and ten patients had the m-bcr (70.5%) and 46 (29.5%) the M-bcr. An IKZF1 intragenic deletion was found in 87/153 (56.9%). Median follow-up was 2.8 years (95%CI 2.6-3.1). All evaluable patients reached CR after a maximum of two cycles. Three patients died during cycle 1 (2 in arm A, 1 in arm B), and 2 during cycle 2 (1 per arm). Most patients received the 4 scheduled cycles (n=143, 91,7%). AlloSCT was performed in 91 patients (58.3%), whereas 41 patients received an autoSCT (26.3%) with no difference in allo/autoSCT rates between arms. A non-inferiority in late MRD response (MRD4) between the two arms was observed (primary endpoint). MMolR was reached in 55/75 (73.3%) and 61/78 (78.2%) of CR patients in arm A and B, respectively, with an estimated 95% CI of difference of -11% to +16% (-9.2% to +20.8% in the ITT analysis treating missing data as failures). At 3 years, overall survival (OS) was 86.0% in arm A versus 74.2% in arm B (p=.08, Figure A). Progression-free survival (PFS) was 79.6% in arm A versus 57.2% in arm B (p=.008, Figure B). Thirty-one patients experienced hematological relapse (8 in arm A and 23 in arm B). Twenty-height out of 31 relapsed patients were tested for the acquisition of BCR-ABL1 mutations, 20/28 (71%) had at least one mutation and 10/28 (36%) had a T315I mutation. At 3 years, the cumulative incidence of relapse (CIR) was 21.3%, significantly higher in arm B than in arm A (30.8% vs 10.6%, p=.007). When analyzing the CIR considering alloSCT as a competing event for relapse, a significant higher CIR was still observed in arm B as compared to arm A (Figure C).
Conclusion. Four cycles of the combined administration of nilotinib and chemotherapy is very efficient for bridging younger adults with Ph-positive ALL to SCT. However, omitting HD-AraC is associated with a higher relapse incidence despite non-inferior levels of BCR-ABL1 MRD4.
Rousselot: Incyte, Pfizer: Consultancy, Research Funding. Chalandon: Incyte, BMS, Pfizer, Abbie, MSD, Roche, Novartis, Gilead, Amgen, Jazz, Astra Zenec: Other: Travel EXpenses, Accomodation; Incyte: Speakers Bureau; Incyte, BMS, Pfizer, Abbie, MSD, Roche, Novartis, Amgen: Other: Advisory Board. Huguet: Novartis: Other: Advisor; Jazz Pharmaceuticals: Other: Advisor; Celgene: Other: Advisor; BMS: Other: Advisor; Amgen: Other: Advisor; Pfizer: Other: Advisor. Vincent: Takeda: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees. Vey: Amgen: Honoraria; BMS: Honoraria; BIOKINESIS: Consultancy, Research Funding; NOVARTIS: Consultancy, Honoraria, Research Funding; SERVIER: Consultancy; JAZZ PHARMACEUTICALS: Honoraria; JANSSEN: Consultancy. Raffoux: PFIZER: Consultancy; CELGENE/BMS: Consultancy; ASTELLAS: Consultancy; ABBVIE: Consultancy. Boissel: Amgen: Consultancy, Honoraria, Research Funding; CELGENE: Honoraria; Servier: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Incyte: Honoraria; SANOFI: Honoraria; PFIZER: Consultancy, Honoraria; JAZZ Pharma: Honoraria, Research Funding. Dombret: Amgen: Honoraria, Research Funding; Incyte: Honoraria, Research Funding; Jazz Pharmaceuticals: Honoraria, Research Funding; Novartis: Research Funding; Pfizer: Honoraria, Research Funding; Servier: Research Funding; Abbvie: Honoraria; BMS-Celgene: Honoraria; Daiichi Sankyo: Honoraria.
Nilotinib as a therapy for PH-positive acute lymphoblastic leukemia

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal